Jersey will develop its own guidelines for which medicines and treatments will remain free for patients, rather than following the UK's National Institute for Health and Care Excellence.
The Health Minister says it might mean some 'minor treatments and non-essential medications' will no longer be available here without charge.
Jersey's TIPP - the Treatment and Interventions Prioritisation Policy - will supersede the UK's NICE guidelines.
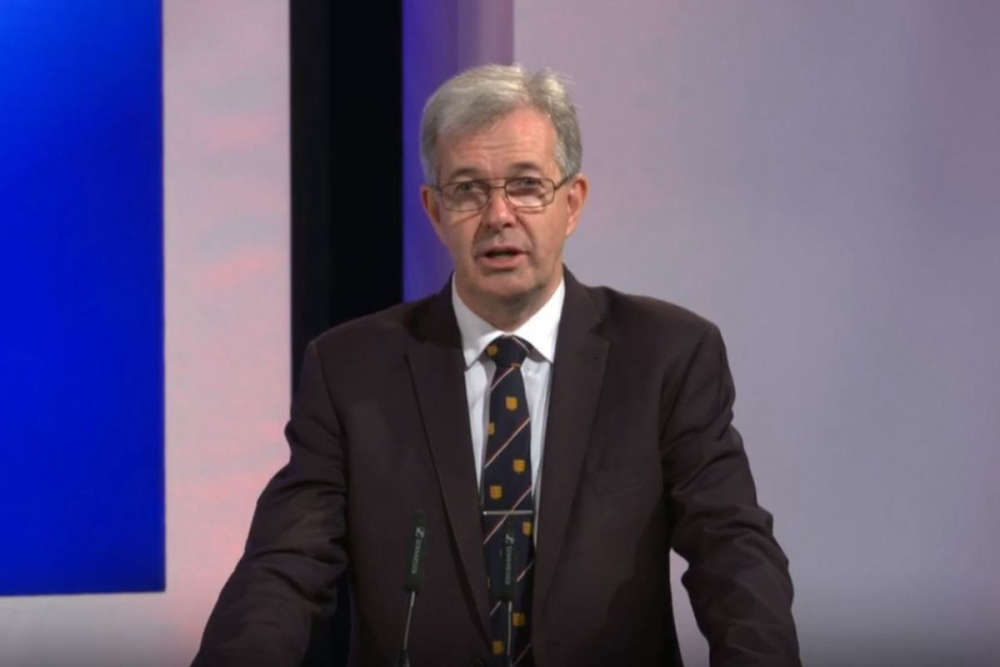
Deputy Tom Binet says Scotland, Wales and Northern Ireland make their own decisions about which medicines are freely available, and that doing the same here will ensure public funding goes on vital services.
He is warning that the island faces 'tough choices' to protect frontline services, with his department facing an £18 million deficit this year.
Decisions will be taken by clinical experts, with those that are of 'significant public interest' escalated to the Health Advisory Board who will make a recommendation to the Minister.
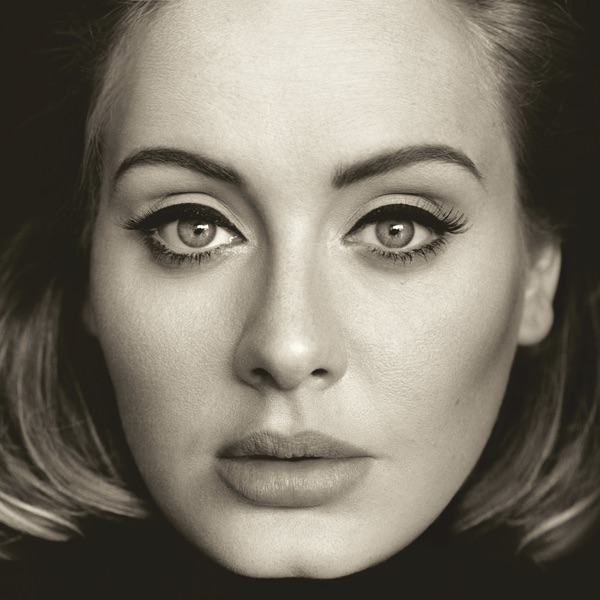
Director of Public Health Professor Peter Bradley told Channel 103 what kind of things might no longer be funded:
"The sorts of things we are thinking about are if you had a short-term, relatively unproblematic illness, you may not get paracetamol prescribed for you.
"In a similar way, if you went to the doctor with varicose veins and you did not like the look of them, you may not get surgery for that reason alone."
 Professor Peter Bradley
Professor Peter Bradley
Deputy Medical Director Dr John McInerney says they are not planning to introduce medication charges:
"We're just going to say 'these are the things we are going to fund that actually work.' If people want to try things that are not licensed or that are easy to obtain at the supermarket - like paracetamol…that seems quite reasonable, so that we can focus our spend.
"There are lots of other drugs we want to pay for. We just need to prioritise which ones are more effective."
The Health Minister says patients should not be concerned about the move to Jersey-specific treatment guidelines.
"All this is is tidying up loose ends. It is formalising a process that has been going on informally in the past.
“It gives much clearer guidance both to the professionals - so they know what they can and can't do as a funded activity - and it gives clarity to the patients as well."
Deputy Binet says health funding pressures are not unique to Jersey, with UK healthcare funding growth running at 3% above inflation.
Longer lifespans, advances in medicine and diagnostic testing, higher clinical safety standards and unhealthy lifestyles are all contributing to a more expensive health service.
The government says costs are rising rapidly:
- The rise in the number of Emergency Department patients needing to be admitted to hospital beds cost an extra £2.4 million in the past year
- The cost of referring patients to the UK and associated travel has gone up by £7 million in nine years from £11.7 million in 2015 to £18.7m in 2024
- The cost of adult mental health placements in the UK has gone up by £2.4 million in four years from £3.4 million in 2020 to £5.85 million in 2024
- The cost of adult social care placements in the UK has more than doubled in four years from £465,000 in 2020 to £988,000 in 2024
Health's proposed budget for 2026 is £381m, £60m more than last year. That includes £12m for preventative and digital healthcare initiatives.
The Minister is also proposing new charges - £77 for attending A&E for a non-emergency and £55 for repeatedly missing outpatient appointments.

 Railway Walk reopens 'several weeks' ahead of schedule
Railway Walk reopens 'several weeks' ahead of schedule
 New bar opening at former Rojo and X site to evolve Jersey's nightlife
New bar opening at former Rojo and X site to evolve Jersey's nightlife
 Former Chief Minister seeks re-election
Former Chief Minister seeks re-election
 Château Vermont to become home to new music campus
Château Vermont to become home to new music campus
 St Saviour break and entry suspect pictured posing on motorbike
St Saviour break and entry suspect pictured posing on motorbike
 'Overstretched' neurology department following under-experienced managers
'Overstretched' neurology department following under-experienced managers
 Channel Islanders asked to report injured or dead seabirds
Channel Islanders asked to report injured or dead seabirds
 'Concerning' e-bike rider not stopping for police
'Concerning' e-bike rider not stopping for police